TPS AND CURRENT COLORECTAL SURGICAL PROCEDURES
Currently, surgical procedures for the treatment of (ODS) can be divided into two broad categories: rectal resection procedures, performed mainly with a transanal approach, and rectal suspension procedures, performed mainly laparoscopically; the latter usually involve the use of biological or synthetic implants. Both categories of procedures, rectal resection and rectal suspension, aim to treat occult rectal prolapse and rectocele, which are considered the main etiopathogenetic factors of ODS.
Without going into detail about the advantages and disadvantages of these two approaches, it is interesting to note that neither of these procedures takes into account either the pathophysiological role that pathological perineal descent can play in ODS or the high frequency with which it occurs.
In fact, a pathological perineal descent is present in more than 75% of patients with ODS and can be seen in 84% of patients who have had failure after any surgical procedure, rectal resection or suspension, performed to treat ODS.
TPS AND PELVIC FLOOR PROCEDURES USED IN GYNECOLOGY
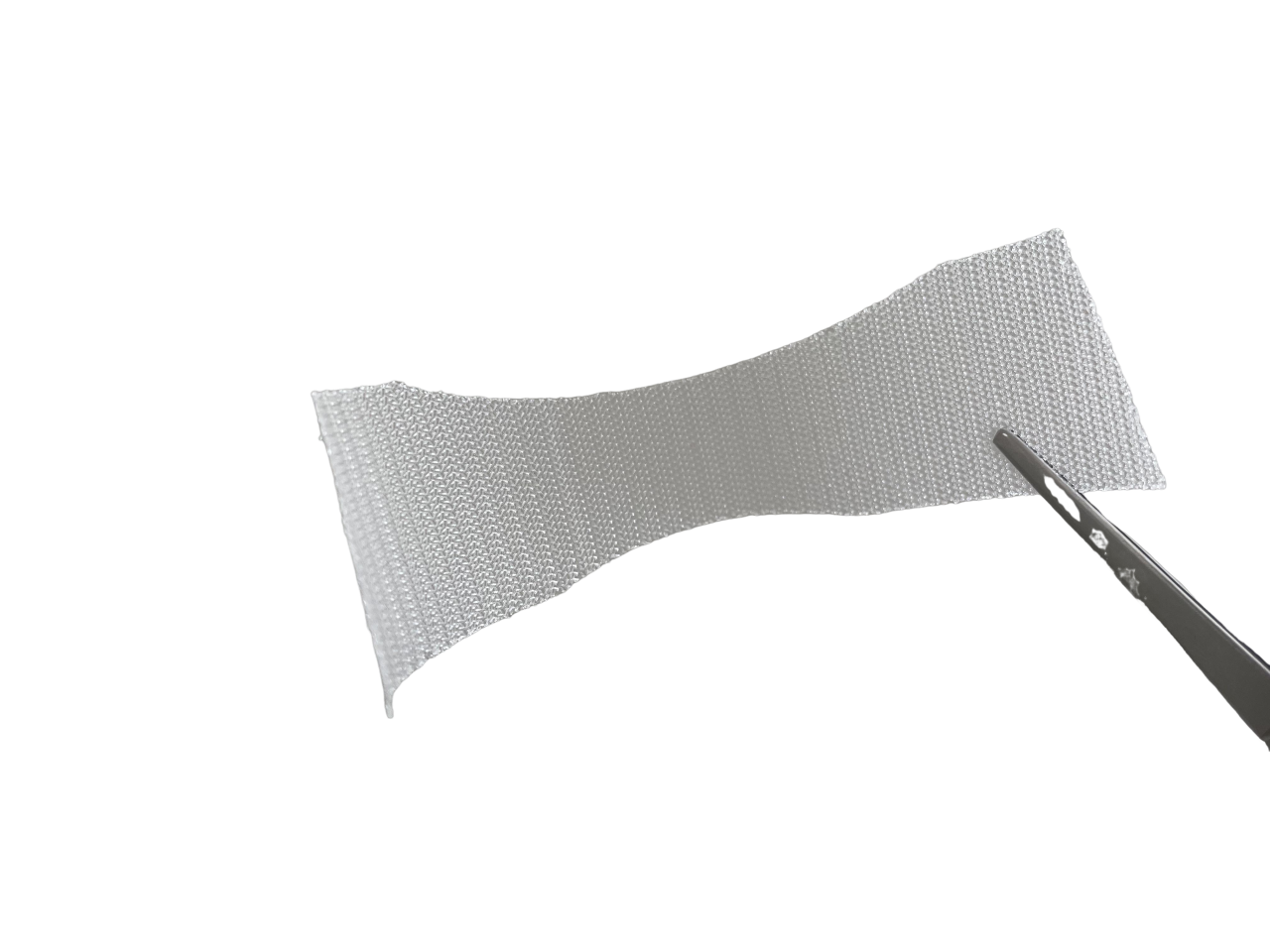
In the last ten years, meshes have been increasingly used in the surgical management of stress urinary incontinence (mid-urethral slings) and pelvic organ prolapse (sacrocolpopexy and transvaginal repairs) in an attempt to improve success rates and increase the longevity of repairs. However, TPS differs from the techniques mentioned above not only in the clinical indication but also in the anatomical location of the mesh (just above the superficial fascia of the perineum). In this position, while creating a supporting element for the pelvic floor, the implant is not in direct contact with the pelvic organs and in no case generates traction/suspension on the latter.
CONCLUSION
TPS is a safe and effective procedure in the treatment of obstructed defecation syndrome associated with the descending perineum. The procedure is simple to perform, easy to learn and with a short post-operative hospital stay.
| KIT CODE | CODES | DESCRIPTION / SIZES | UNITS |
| TPS | AM0311 | Polypropylene mesh, pre-shaped, Vertical Cut, 3 cm x 12 cm | 1 |
| PS028HHAC | Filbloc Permanent for ENDO 360° – 22 mm – Non-absorbable unidirectional barbed polypropylene suture with final lock, USP 2/0, length 20 cm |
4 |
 OTHER
OTHER